In the structure of the pathology of the osteoarticular system, osteoarthritis occupies a leading position - about 70% of cases fall into its share. A similar problem is more often faced by people after 50 years, but the initial signs of the disease appear even in young people. This disease is of serious medical and social importance, because in many cases it becomes the cause of functional insufficiency in working age.
Many people know about such a pathology as arthrosis of the joints, but not every patient understands why it develops, how it manifests itself and what is required to fight the disease. And increased awareness and attention can prevent harmful changes from occurring and progressing.
The reasons
Osteoarthritis is characterized by the development of degenerative-dystrophic processes in all joint tissues: cartilage, subchondral bone, ligaments, muscles and tendons. The disease is considered one of the "companions of aging" because it often affects older patients. But the age factor is far from being the only cause of degenerative joint disease. The origin of the disease is quite heterogeneous and is due to both external and internal types of pathological effects on the body.
For each patient there are certain risk factors that contribute to the appearance of joint pathology. Therefore, the causes of arthropathy combine the following conditions:
- Hard physical work.
- Inaction.
- Traumatic injuries.
- Joint dysplasia.
- Inflammation (arthritis).
- Overweight.
- Estrogen deficiency in menopause.
- Diseases of the thyroid gland.
- Consequences of joint operations.
- Heredity.
As you can see, the development of articulation is mediated by heterogeneous factors, which in most cases are mechanical or exchangeable in nature. In this case, the lifestyle of the patient and his profession are of little importance, because loaders, manual workers and athletes often suffer from arthropathy.
The causes of arthropathy are quite different, characterized by a local effect on the joints and a general effect on the body.
Development mechanism
The normal functioning of the joint is ensured by the harmonious work of all its structures. But the main component of every joint is cartilage. Provides shock absorbing function and resists pressure on the joint. Cartilage tissue consists of cells (chondrocytes) and a matrix, the main substances of which are proteoglycans and collagen.
If the load on the joint exceeds the permissible, then first there are structural disorders in the cartilage. The proteoglycans that hold the collagen strands together are lost, which increases the sensitivity of the tissue to external influences. Destruction processes begin to override synthesis. This is facilitated by the reduction of cartilage trophism when the synovial fluid contains an insufficient amount of nutrients. The imbalance of tissue renewal is supported by inflammatory reactions and hormonal disturbances.
All this leads to a thinning of the cartilage, it becomes rough and loses its elasticity. Due to the growth of the underlying bone tissue, the joint space narrows and osteophytes are formed - border growths. The synovial membrane thickens, ligaments thicken and shorten, and muscle function is disrupted.
Pathological processes in the joint develop gradually, but do not pass without a trace. Disorders of cartilage and other structures inevitably affect the clinical picture of osteoarthritis.
Classification
Arthritis, like other diseases, has certain varieties. This should be taken into account in the clinical classification of the disease. The pathology is primary when it develops in healthy joints or secondary if it occurs in the context of other diseases. In the event that the cause cannot be established, they speak of idiopathic osteoarthritis. Depending on the number of joints involved, the following varieties are distinguished:
- Single joint.
- Oligoarthritis - no more than 2 joints are affected.
- Polyarticular - involves 3 joint groups.
If the pathological process has a generalized character, then we can talk about the defeat of almost all joints of the body, including the spine, where spondyloarthritis is observed. In this case, the disease can progress to a nodular or nodular form.
It is important to understand what processes occur in the joint and adequately assess their severity. Therefore, be sure to consider the stage of articulation. It does not depend on the cause and is determined by pathological changes in the synovial tissues:
- Stage 1 - inflammation of the synovial membrane, loss of the ability of the cartilage to withstand the load.
- Stage 2 - cartilage tissue destruction, bone growths, synovial sac dystrophy.
- Stage 3 - bone deformation, contractures, joint instability.
The presence of signs of inflammation should also be reflected in the classification. Therefore, osteoarthritis is distinguished with and without arthritis. In addition, the functional state of the joint is important, which is determined by the degree of deficiency:
- 1 degree - temporary restriction of operation.
- Grade 2 - disability.
- 3 degree - the inability to care for oneself.
All these features should be reflected in the diagnosis of osteoarthritis, as they are important for subsequent treatment.
Symptoms

Among articular pathology, the symptoms of arthropathy have quite tangible specificity. They develop gradually, but progress steadily, leading to a limitation of the patients' physical activity. Therefore, it is especially important to suspect the disease in time to be able to stop its development, as well as to prevent complications.
When contacting a doctor, first of all, patient complaints are analyzed. And mostly people worry about joint pain. But with arthropathy, unlike other pathologies, such as arthritis, they have the following character:
- Mechanical - occur in the background of the load and decrease at rest.
- Onset - the onset of pain is associated with the onset of movement (walking).
- "Articular mouse" - periodic acute pains with joint blockade, caused by a violation of the synovial membrane between the cartilaginous surfaces.
At first, patients may experience only vague discomfort in the joints, accompanied by a feeling of fatigue. But over time it develops into pain. And if in the initial stages it worries after a load, then in the future - during movement and in advanced cases it becomes stable, remaining even at rest and at night.
In addition to pain, patients have other joint symptoms. They are both subjective and objective in nature, including the following characteristics:
- Stiffness in the joints in the morning not more than 30 minutes.
- Crepitus when moving.
- Deformation of the periarticular area.
- Mobility restriction.
With arthropathy of the hands, during the examination, one can observe characteristic formations in the region of the proximal and distal phalanges - Bouchard and Heberden nodules. The sensation of the affected joints is often painful. If contractions are formed, then there is a fixation of certain parts of the limbs more often in a bent position.
The intense nature of osteoarthritis leads to a significant reduction in the level of physical activity of patients, which implies a reduction in their quality of life.
Diagnostics
To understand why the clinical picture develops, it is necessary to confirm the pathology of the joints. This can be done by carrying out the necessary diagnostic examination, which includes instrumental and laboratory methods. First of all, they try to see structural changes in the affected areas, assess their severity and prevalence. It is also necessary to determine the metabolic disorders in the body, which have become a favorable background for the appearance of joints. Therefore, the research complex consists of the following activities:
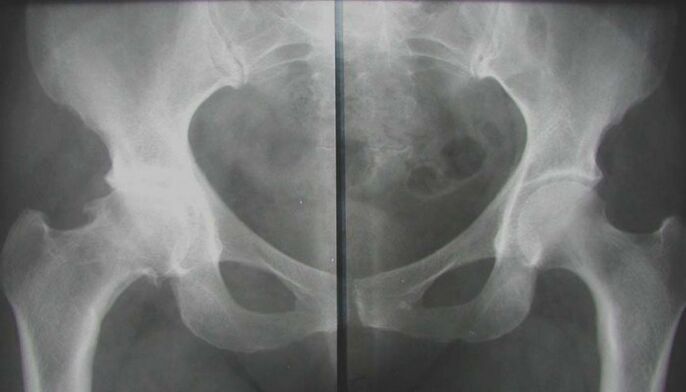
- X-ray.
- Magnetic resonance imaging.
- Ultrasonic process.
- Arthroscopy.
- Biochemical blood tests (hormone spectrum, inflammatory markers, calcium metabolism, rheumatic tests).
After the examination, a consultation with an orthopedic-traumatologist will be required, which will help to formulate the correct regular treatment for each patient.
Treatment

It is necessary to treat arthrosis of the joints comprehensively. This means that all available therapeutic agents are used to alleviate the patient's condition. But you must understand that their effectiveness directly depends on the time of treatment. With advanced forms of the disease, conservative measures will help little. An intense and lasting effect can be achieved with timely treatment. The following methods are used to treat osteoarthritis:
- Medical treatment.
- Physiotherapy.
- Physiotherapy.
- Massage.
- Mode.
Which funds are suitable for a particular patient, the doctor decides. The choice is made based on the results of the examination and the individual characteristics of the organism.
The best result of the treatment can be achieved if the correction begins in the initial stages of the disease, when the first symptoms have just begun to appear.
General recommendations
Since the development of degenerative changes in the joints is caused by an increased load, it is first necessary to reduce the mechanical effect on the cartilage tissue. To do this, you should stop wearing heavy, intense sports training. To unload the joint, any method is suitable - from walking with a cane to special fixing braces. But it is impossible to completely abandon movements, physical activity should be dosed. Walking for short distances, swimming are useful.
Proper nutrition plays an important role in correcting joint changes. Nutrition helps to improve the condition of the cartilage, but it is also the main component in the fight against excess weight. Patients are advised to consume lean meats and poultry, fish, cereals. you need to enrich the diet with fresh vegetables and fruits, herbs. But in return, you should refrain from smoked, spicy, fatty foods, marinades and pickles. It is better to pay attention to foods rich in collagen fibers, elastin and gelatin: meat jelly, hashish, dishes with aspicia, fruit jelly.
Medical treatment

Traditional treatment for osteoarthritis begins with medication. Using various drugs, it is possible to eliminate not only the symptoms of the disease, but also to affect the mechanisms of its development. This is especially important in chronic degenerative joint pathology, when it is necessary to achieve a structure-modifying effect on cartilage tissue. The following drugs are generally recommended:
- Non-steroidal anti-inflammatory.
- Carboprotectors.
- Vascular.
- Vitamins and antioxidants.
- Metabolic (estrogens, thyroid hormones).
With severe pain in arthrosis, intra-articular injections of glucocorticosteroids can be given. But such treatment should be short-term, because with prolonged use, hormonal drugs have the opposite effect - they stimulate dystrophic processes. Systemic treatment should be combined with local drugs.
Medicines for osteoarthritis are taken on the recommendation of a doctor and under his control. Independent use of any drugs is not allowed.
Physiotherapy

Methods of natural influence help to eliminate the acute signs of joint pathology. Together with drugs, they can reduce the severity of pain and inflammation and also stimulate biochemical processes in the cartilage itself. In the complex treatment of arthropathy, the following procedures are used:
- Electrophoresis.
- Ultrasound therapy.
- wave therapy.
- Magnetic therapy.
- laser treatment.
- Mud and hydrotherapy.
Such methods affect not only the joint, but also the surrounding tissues. This contributes to the activation of blood circulation, the improvement of food processes and the weakening of muscle contractions. Many elements of spa treatment have a general health-improving effect. But at the same time, we must not forget the contraindications to physiotherapy: infectious diseases, tumors, cardiovascular pathology, kidney failure, bleeding, serious condition of the patient.
Physiotherapy
An important aspect of the non-drug treatment of osteoarthritis is exercise therapy. It is known that the metabolism of cartilage tissue has a clear dependence on the mechanical factor. But its power must be sufficient. Only then do processes of growth prevail over destruction. Therefore, gymnastics is indicated for all patients with joint diseases. But for each person, his own set of exercises is developed - taking into account the localization and severity of the damage, as well as the general condition of the body.
During classes, pain should not be allowed. The exercises are done at a slow pace and only after the acute symptoms have been eliminated. Avoid sudden and wide movements that may cause discomfort. Physical education should be done under the supervision of a doctor and after you have acquired the necessary skills, you can start exercises at home.
Therapeutic gymnastics is an integral component of the correction of degenerative-dystrophic processes in the joint. Only regular lessons have a positive effect.
Massage

To improve the condition of the musculoskeletal system, massage sessions are performed. Manual impact on the joints allows you to achieve relaxation of spasmodic muscle groups, stimulate blood circulation in soft tissues and prepare them for active exercises (before therapeutic exercises). Classic massage includes the following elements:
- Caressing.
- Pulverization.
- Kneading.
- pressure.
- Ironing.
It is often combined with passive movements in the affected joints. The duration of treatment is determined by the doctor and can be from 7 to 15 sessions.
Mode
If the advanced stages of osteoarthritis do not allow to achieve the desired result from conservative measures, then there is a need for surgical treatment. Its essence is the replacement of the joint with an artificial one - arthroplasty. This operation is performed in an open manner and with general anesthesia. After its completion, you must undergo rehabilitation, which begins as soon as possible. And as a result of surgery, the patient can completely get rid of arthropathy and return to an active life. It is true that the feature is not available to everyone.
Osteoarthritis is a common problem that requires an early and active solution. In order not to start the disease and to be able to hope for the success of conservative measures, treatment should be started as early as possible. This will avoid exacerbations, prevent the progression of changes in the joints and restore the functional abilities of the musculoskeletal system as much as possible. Otherwise, surgical correction should be considered.


























